As COVID-19 cases in many U.S. states like Florida and Texas are surging, the total U.S. case rates are doubling from the infection peaks seen in March and April. At the same time though, mortality is not nearly increasing at the same rate as infections. How can this phenomenon be reconciled? Dr. Brian Abrahams, our Co-Head of Biotechnology Research, shares five factors contributing to this trend from his research report “COVID-19 is Spiking, but Why Not the Deaths? Exploring the Implications” published on July 17, 2020.
An intrinsic lag time and shifting methodologies may account for an apparent lower proportion of COVID-related deaths relative to the infection spike.
The median time course from symptom onset to death is roughly 15 days for individuals less than 65 years old. Administrative issues such as COVID-19 death certificates being coded by hand, a shift away from the CDC controlling the data, and different state reporting standards, can lead to a delay in counts ranging from one to eight weeks. With all those limitations, on average the data suggests that the time from diagnosis to recorded death is approximately three weeks.
An increase in testing may capture previously unreported cases to some degree.
A greater quantity of tests has often been cited as an explanation for the apparent resurgence of the pandemic, along with expanded access to testing and contract tracing, general disease awareness, and increased detection of earlier infections and asymptomatic cases. However, daily testing capacity has only nearly doubled since June 1, while cases have increased more than three times in the same time frame. Therefore, it is unlikely to be the sole explanation for the lower apparent mortality rate.
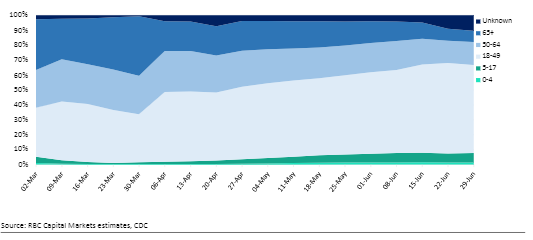
Lower-risk populations contracting the disease may blunt mortality.
Anecdotally, younger patients are more likely to be engaged in riskier close-contact activities, so it is possible that a majority of infections are within a demographic most likely to survive. However, this assumption is not necessarily ironclad. If presumably lower-risk individuals begin to spread the disease to higher-risk contacts (i.e., a family member with a pre-existing condition), this could contribute to a "second wave" of COVID-related hospitalizations and deaths.
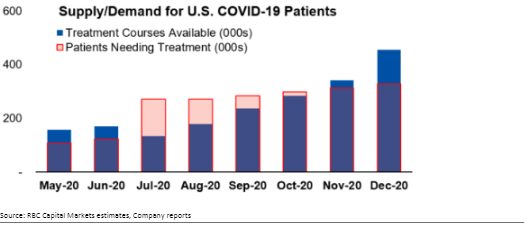
New treatment options, such as Remdesivir, are having a modest but real effect.
In a randomized controlled trial by the National Institute of Allergy and Infectious Diseases, Remdesivir was shown to accelerate recovery by 32% and reduce mortality by 30%. Although modest, these effects are real and could contribute to a noticeable reduction in mortality on a population level. But is there enough Remdesivir to go around? We estimate there could be a meaningful supply shortage in July through September before production catches up to demand by October and through the winter months.
The potential for viral mutations attenuate disease severity.
There is convincing scientific evidence that SARS-COV-2 has mutated, with the D614G mutation in the spike protein being increasingly prevalent. Studies of this mutation have shown that it increases infectivity nine-fold in the lab, and there is clear evidence that the D614G mutation is more prevalent in newer outbreaks than from the start of the pandemic. While so far there is no evidence that this mutation is deadlier, the virus can accumulate additional mutations with unknown functions, so it will be important to continue to monitor this.
Dr. Brian Abrahams authored the research report “COVID-19 is Spiking, but Why Not the Deaths? Exploring the Implications” published on July 17, 2020. For more information about the full report, please contact your RBC sales representative.
